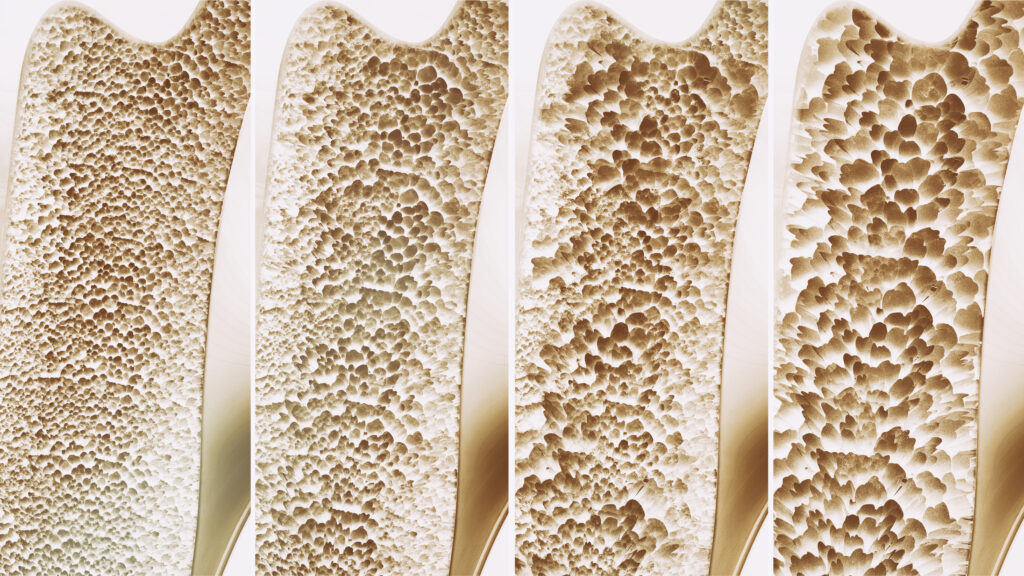
Osteoporosis is a condition characterized by the weakening of bones, making them fragile and more likely to break. It is often referred to as a “silent disease” because it progresses without obvious symptoms until a fracture occurs. This condition is most common in older adults, particularly postmenopausal women, but it can affect anyone. Fortunately, there are various treatments and medications available to manage osteoporosis and reduce the risk of fractures.
1. Lifestyle Changes
Before diving into specific medications, it’s important to highlight the role of lifestyle changes in managing osteoporosis. These changes can help slow bone loss and improve overall bone health.
- Diet: A diet rich in calcium and vitamin D is crucial. Calcium supports bone structure, while vitamin D improves calcium absorption. Foods like dairy products, leafy greens, and fortified cereals are good sources of calcium. Sunlight exposure and foods like fatty fish can help with vitamin D intake.
- Exercise: Weight-bearing exercises, such as walking, jogging, and resistance training, are beneficial for bone health. Regular physical activity helps maintain bone density and strength.
- Lifestyle Habits: Quitting smoking and reducing alcohol consumption can also improve bone health, as both smoking and excessive alcohol intake are linked to bone loss.
2. Medications for Osteoporosis
When lifestyle changes are not enough to manage osteoporosis, doctors may prescribe medications. These medications either slow down bone loss or promote bone formation.
a. Bisphosphonates
Bisphosphonates are the most commonly prescribed medications for osteoporosis. They work by slowing the rate at which bone is broken down in the body, which helps maintain or even increase bone density. Common bisphosphonates include:
- Alendronate (Fosamax): Taken once a week or daily.
- Risedronate (Actonel): Available in daily, weekly, or monthly doses.
- Ibandronate (Boniva): Taken monthly as an oral tablet or quarterly as an injection.
- Zoledronic acid (Reclast): Administered as an annual intravenous infusion.
b. Denosumab (Prolia)
Denosumab is a monoclonal antibody that slows down bone resorption, similar to bisphosphonates. It is administered via injection every six months. Denosumab is often prescribed to individuals who cannot take bisphosphonates or who do not respond well to them.
c. Hormone Therapy
Hormone-related therapies can be effective, particularly for postmenopausal women.
- Estrogen Therapy: Estrogen helps maintain bone density. However, due to the risks associated with hormone replacement therapy (HRT), such as increased risk of breast cancer and cardiovascular issues, it is generally recommended for women who also need HRT for menopausal symptoms.
- Selective Estrogen Receptor Modulators (SERMs): Raloxifene (Evista) is a SERM that mimics estrogen’s bone-preserving effects without some of the risks associated with estrogen therapy. It is particularly useful in preventing spine fractures.
d. Parathyroid Hormone Analogues
Teriparatide (Forteo) and Abaloparatide (Tymlos) are synthetic forms of parathyroid hormone that stimulate new bone formation. These medications are typically prescribed for people with very low bone density or those who have experienced fractures. They are administered by daily injection for up to two years.
e. Romosozumab (Evenity)
Romosozumab is a newer medication that both increases bone formation and decreases bone resorption. It is given as a monthly injection for 12 months. Due to a potential risk of heart attack or stroke, it is typically prescribed for those who are at high risk for fractures and have no history of cardiovascular disease.
3. Monitoring and Follow-Up
Treating osteoporosis is an ongoing process that requires regular monitoring. Bone density tests, typically done using dual-energy X-ray absorptiometry (DEXA), are used to assess the effectiveness of treatment. Your healthcare provider may adjust your treatment plan based on these results.
4. Managing Osteoporosis with Combination Therapy
In some cases, doctors may recommend combining medications to optimize treatment. For example, a patient might start with a bone-building medication like teriparatide and then switch to a bisphosphonate to maintain the bone density gains. This approach is often used in individuals with severe osteoporosis or multiple fractures.
Osteoporosis is a serious condition, but with the right treatment plan, the risk of fractures can be significantly reduced. Lifestyle changes play a crucial role in managing the disease, but medications are often necessary to effectively maintain or improve bone density. If you have osteoporosis, it’s important to work closely with your healthcare provider to choose the best treatment plan for your specific needs. Regular monitoring and possibly adjusting your treatment over time will help you maintain bone health and reduce the risk of fractures.